
Inside Out: The Intertwined Bond
Have you ever experienced a feeling of butterflies during a nerve-wracking situation? Or that your digestion has worsened after a stressful day? Well, these are just a glimpse of the deeply rooted connection between your gut and your mind.
Throughout this article, we’ll step into the intriguing realm of the gut-brain axis, where your belly and brain are more intertwined than you first think. We will also explore how factors like diet, stress, and gut microbiota can not only affect our physical health but also our mood regulation, cognition and responses. Understanding this connection opens new avenues for treating conditions like anxiety, depression, and even neurological disorders through gut-targeted interventions.
What is it?
The gut-brain axis encompasses a network of connections between the central nervous system (CNS), enteric nervous system (ENS), endocrine system, and the immune system. However, we are concerned with how the two systems are linked, specifically through the vagus nerve network. This fibre is a communication highway that runs down from the brain stem, branching out to innervate various organs, including the heart, lungs, gastrointestinal tract, and intestines.
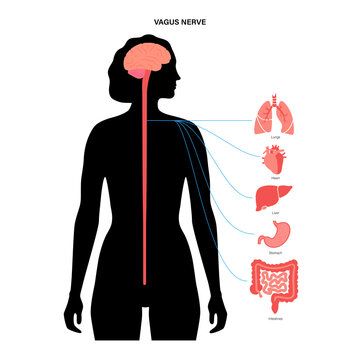
These connections allow an almost instant reaction to free-flowing pieces of information within linked organs. In other words, you can think of this nerve as a de-restricted location on the German Autobahn, where cars can go as fast as they please with no speed limitations, with each junction being a separation from an organ.
Examples of such messaging are the heart asking the brain to regulate blood pressure, the lungs requiring more O2 and CO2 so requests the brain to increase breath rate, and the stomach releasing ghrelin when requiring sustenance. This is just a drop in the ocean of all the messaging our organs send up. In fact, our most recent search suggests that the vagus nerve likely processes millions of messages daily.
However, not only can organs send pieces of information to the brain, but also vice versa. Meaning that the brain also sends information to the connected organs when in certain, usually stressful, situations. This connection is what we mean when discussing the gut-brain axis.
Finally, we should discuss exactly what the ‘gut’ is. This phenomenon isn’t just one physical organ as some people seem to assume. In fact, it is based on the organs that have priority within the digestive system. For example, when people refer to ‘the gut’, they mostly acknowledge the stomach and intestines, noting the distinct interplay with how our food is absorbed, digested and stored, and also how our immune system functions.
As food enters our stomach it is broken down into smaller peptides by the gastric juices produced inside the lining. As these peptides are made smaller, they enter the intestinal tract where the nutrients are absorbed and the rest is left as waste. These nutrients are transported throughout the body to provide energy and support various physiological functions. Meanwhile, the undigested peptides move through the colon as waste products, where water is absorbed and solid waste is formed.
Now, a lot of you may be wondering where the highly contested concept of your gut microbiome comes in. Essentially, this biome lives within the large intestines and the colon. Their direct occupation is to break down certain food components that our digestive enzymes can’t fully process, such as complex carbohydrates and fibre. They also help with the absorption of certain vitamins like B and K and produce beneficial by-products that our body can utilise as energy.
In essence, the gut-brain axis is a complex network connecting multiple systems, allowing for bidirectional communication between both. This communication facilitates the free flow of information that allows the body to react to certain stimuli.
The Importance
But exactly how does that affect our fitness journey? Well, without eating so-called “gut-beneficial foods” (more on this later), your body cannot fully digest and manipulate the calories into energy. In fact, your gut is the primary driver of bodily inflammation. If it is not treated correctly, you could be left with signs of eczema, acne, swelling, and even psoriasis. However, as mentioned before, the vagus nerve also has a role to play. Stressful stimuli send messages down the body and into the gut, which can also cause inflammatory responses such as the ones listed. Even concepts like anxiety, sleep deprivation, depression, fight or flight, and inactivity can cause similar gut-related responses.
So how do we make sure that our gut lives in a positive manner, to try and make sure we avoid as much inflammation as possible? Well, the answer may surprise you. Unfortunately, a lot of foods that we eat contain substances called anti-nutrients. These are compounds that hinder the digestion and absorption process within the intestines and colon.
Foods with the highest anti-nutrient profile per weight are legumes, whole grains, nuts and seeds, leafy greens, and cruciferous vegetables. The foods with the least anti-nutrients are animal products, dairy, fruits, and non-cruciferous vegetables.
This might be surprising to many. But let me explain. When you see an animal, take a dog, for example, it has many ways to protect itself. This being claws, teeth, speed, strength and power. However, when you think of a leafy green substance like a spinach leaf, it doesn’t have any of those. In fact, the only way a piece of spinach can stop itself from being eaten is through releasing toxic products when damaged or feeling endangered. These oxalates contain very tiny sharp crystals that can line the urinary tract causing kidney stones. Similar effects on your organ health can be seen with broccoli’s goitrogens, an almond’s phytic acid, and a kidney bean’s lectin.
Not only this, but foods that are difficult to digest have a similar effect. Examples of these are highly refined sugars, low-fibre content carbohydrates, artificial stabilisers and additives, and trans fats. All of which are found in highly processed foods, takeaways, seed oils, and even protein products.
Now, to set the record straight, the foods we have the most difficulty digesting are not meat. I have heard time and time again, that because meat takes longer to digest, this must mean it is difficult for our body to process. This is in fact not true. It is actually the opposite. Meat takes longer to digest because of its higher dietary fat content, with dietary fat containing 7 units of energy per gram, while protein and carbohydrates contain 4. This means per gram, dietary fats contain the most energy for our body, so take the longest to fully process.
Mental Health Impact
Our physical well-being isn’t the only phenomenon affected by our gut. As we know, the vagus nerve runs information up and down, allowing any stressors felt by either organ to be communicated. Therefore, not only can anxiousness, depression, and stress affect the gut, but mismanaged microbiota can contribute to such conditions.
The gut microbiota plays a significant role in neurotransmitter production. Some of the most important types being, serotonin, dopamine and GABA. An imbalance within this biome causes deregulatory production, leading to the ineffective release of these transmitters. When I said “significantly”, the intestines produce 90% of the body’s serotonin. Insufficient serotonin levels are correlated with dysregulated mood, appetite, and sleep. It also has been correlated with quite a contested condition called ‘Irritable Bowel Syndrome’ (IBS), but that’s for another day.
The same can be said for dopamine and GABA release. Dopaminergic neurons and receptors are present within the gut. Ineffective production of dopamine and GABA is correlated with poor gastrointestinal motility (constipation), and impaired immune function.
Practical Tips
I understand this is a lot of information to take in, and it can seem quite bewildering how one organ can alter our manner of living. But, simple lifestyle changes negate 99% of all worries regarding our digestive tract.
First, minimise heavily refined sugar intake. These consist of sugars that have their nutrients and molasses stripped away to encourage a sweeter taste. Unfortunately, sugars like this dysregulate the bacteria within our gut by increasing the opportunistic pathogens. A high level of these bacteria lead to impaired neurotransmitter production, and inflammatory responses whilst they’re exterminated.
Second, reducing emulsifier consumption. Emulsifiers are substances that help mix two or more ingredients that normally cannot go together. For example, we would need an emulsifier to enable the mixture of water and oil, as they naturally repel one another. The most common type of emulsifier within our foods is lecithin, a binding agent derived from soybeans. Research has shown these to cause inflammatory responses within the gut
Third, decreasing artificial flavouring and sweetener intake. Essentially, these enhancers are cost-effective ways to include a certain taste or aroma in your products. Almost every type of processed food contains some sort of artificial flavour. These have been seen to cause inflammatory responses, leaky gut, gut barrier impairments, and changes in gut hormone secretion
Finally, stop the consumption of sugar alcohols like sorbitol, and xylitol. The concept behind these sugars is they are meant to provide the extremely sweet taste, but not cause any blood glucose spikes. However, consumption has been correlated with gastrointestinal discomfort, impaired gut hormone secretion, and an increase in pathogenic bacteria within the gut.
In conclusion, the intricate relationship between our gut and brain, also known as the gut-brain axis, suggests a profound impact on our mental and physical well-being if digestive health is not sound. From mood regulation to immune function, the communication between these two systems influences every aspect of our lives. By starting to understand this connection and the influence our dietary lifestyle has, we can promote interventions for many life-altering conditions.
Leave a comment