We’ve all heard about the health crises surrounding the rising numbers of cardiovascular disease, diabetes, cancer, and mental health struggles. But one of the most concerning issues, rarely discussed, is the extremely rapid reduction in men’s testosterone (T) levels. Testosterone, crucial for the development of physical, emotional, and social male characteristics, plays a vital role in everything from muscle mass to mood regulation, fertility, cognitive function, and even red blood cell production and bone density. While attention is often focused on more visible health concerns, this rapid decline is having a profound impact, not just on the male population but on society as a whole. Some of these effects include an increased risk of depression, fatigue, reduced sperm count, and even metabolic disorders. Unfortunately, this issue is seldom addressed openly and is sometimes dismissed, despite its significant impact on men’s (and women’s) quality of life.
This decline is extremely alarming. Current research shows that the average total testosterone level in fertile men is about 30% lower than it was just two decades ago. This extraordinary drop is unprecedented in modern history. The implications are staggering: a generation of men with significantly diminished physical and emotional vitality, along with the associated health risks.
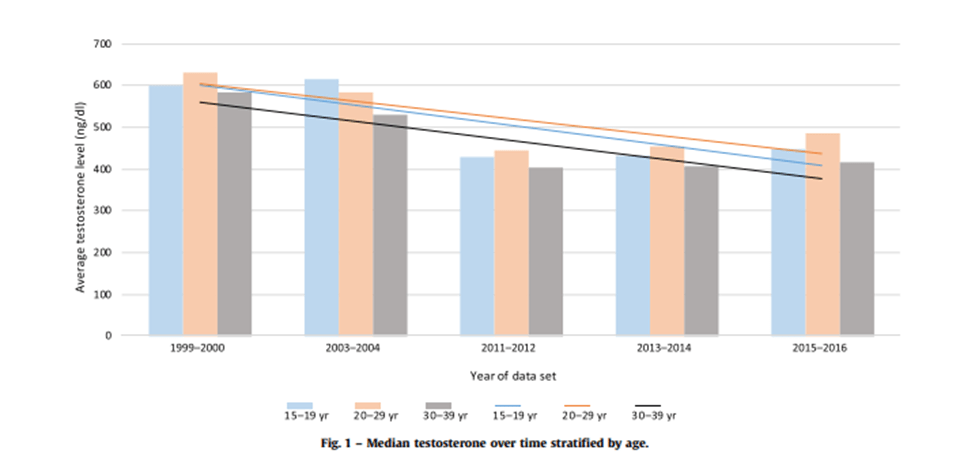
With testosterone levels in such decline, we are witnessing a rise in health problems traditionally linked to low testosterone, such as cardiovascular disease, mental health disorders, and poor fertility. The pressing question is: why are men’s testosterone levels dropping so dramatically, and what can we do about it?
Firstly, we need to understand the cause of this rapid decline over just two decades. Several factors are understood to be primary contributors, some of which are difficult to control. Environmental toxins are known to play a major role. Phthalates, Bisphenol A (BPA), and pesticides have all been persistently linked with increasing estrogenic properties in humans and animals. These substances are commonly ingested through contaminated food, absorbed through skin contact, or inhaled from the air. What’s worse is that men encounter these endocrine disruptors several times a day! For instance, pesticides are found in most of our fruits, vegetables, and grains. BPA is present in metal food linings, canned beverages, plastic containers, water bottles, and receipts, while phthalates are found in most perfumes, deodorants, lotions, shampoos, and even detergents. The prevalence of these disruptors is so extreme that pesticides are present in 80% of our produce, phthalates in 70%, and BPA in up to 90%!
This means that every time you shower, eat fruit or vegetables, drink water, go shopping, try to make yourself smell appealing, or use moisturiser, you’re encountering a substance that could alter your hormonal balance and contribute to the decline of testosterone. This constant exposure creates a cumulative effect, making it nearly impossible to avoid these harmful chemicals in everyday life.
Additionally, lifestyle factors play a significant role. Chronic stress, mismanaged diet, and sedentary habits all contribute to a decrease in testosterone. Chronic stress is highly associated with the overproduction of cortisol – the body’s “stress hormone”. Its impact on testosterone is direct, as it inhibits production in the testes. Chronic stress also triggers high levels of inflammation, specifically ROS (reactive oxygen species) accumulation, which further impacts testosterone production.
Another lifestyle factor that can severely affect men’s testosterone levels is a mismanaged diet. I prefer the word “mismanaged” in this context because labelling a diet as “poor” can be subjective. When it comes to correlating with testosterone levels, objective evidence is needed. For instance, a diet low in cholesterol means testosterone cannot be synthesised (which may be the origin of the term ‘soy boy’). Testosterone is a steroid hormone that requires pregnenolone, a hormone precursor, which can only be converted from cholesterol. Additionally, a diet that leads to abdominal obesity increases the activity of the aromatase enzyme, which converts testosterone into oestradiol – a form of oestrogen.
Finally, excess body fat, as mentioned earlier, causes a reduction in testosterone. An individual with a sedentary lifestyle suppresses the HPG axis, AMPK, and myokines, all of which help produce and regulate testosterone. A man who does not exercise, has abdominal fat, follows a diet low in red meat and eggs, and regularly uses personal care products laden with chemicals will likely have testosterone levels below average.
But why is this important? From what we’ve been told, testosterone isn’t that important. It supposedly only produces toxic masculinity, crime, aggressiveness, and high libidos. So surely a reduction in testosterone is beneficial for society? This could not be further from the truth.
If this were true, why have instances of sexual assault, stalking, and other crimes against women dramatically risen? If male testosterone scarcity were a beneficial circumstance, then all XY-dominated crimes would be dropping, not rising. The reason this is not the case is that men with lower testosterone levels are more likely to exhibit “toxic masculinity” traits – but that’s for another article.
Since this reduction began, we’ve seen an inverse relationship with obesity, fat mass, cardiovascular disease, depression, anxiety, and even suicide. Furthermore, we’ve seen a significant decline in fertility, which could be contributing to birth rates dropping below replacement levels. Such an issue is detrimental to wider society because it is linked to a cascade of health problems, placing unnecessary strain on our healthcare system. This strain leads to increased costs, burdening both public and private sectors. As more resources are diverted to managing conditions correlated with lower testosterone, other healthcare services may suffer from underfunding.
Additionally, the drop in fertility affects not only population numbers but also family structures. With fewer children being born (though not all of the blame can be attributed to low testosterone levels), we are living below replacement level. If this issue is not addressed, it could lead to long-term social, economic, and demographic difficulties that would affect the prosperity of society. Without intervention, we could face labour shortages, decreased tax revenue, and a stagnating economy – all while our healthcare system remains strained.
So, what can we do about it? Firstly, there needs to be policy intervention to reduce exposure to environmental toxins. Whether this takes the form of tax benefits for BPA-free products or forcing farms to reduce pesticide usage, any action that reduces contact with these endocrine disruptors will help. Secondly, we need to change our dietary recommendations. Currently, we are told that cholesterol is bad and will cause heart disease, but this is not entirely true. We need to inform people that a diet including clean red meat and eggs is beneficial. Additionally, educating men about the importance of minimising processed foods and reducing abdominal fat will enable better lifestyle choices. Thirdly, we need to promote physical activity more effectively. Rather than just encouraging people to go to the gym, we need stronger incentives, perhaps through increased fitness programmes in schools to embed physical activity in our culture, or through tax credits or insurance premiums for those who attend regularly. Finally, we need to de-stigmatise testosterone replacement therapy, which is often seen as something only for bodybuilders. Most men living with below-average testosterone levels would benefit from medically supervised hormone replacement to sustain normal living.
Addressing this crisis requires a multi-faceted approach involving policy intervention, dietary changes, and the promotion of physical activity. Without decisive action, we cannot expect this health crisis to change. As a society, we must de-stigmatise the conversation surrounding men’s hormonal health. Men should get their testosterone levels checked regularly to ensure they are addressing potential health issues before they become more severe. If we do not act, the physical, mental, and societal costs will continue to rise, affecting not just men but our entire community.
Leave a comment